Devices already on the EU market
A large part of the medical apps will be categorized in a higher risk class
Fact
The MDR has a separate classification rule for medical software (annex VIII, rule 11). It states that software intended to provide information which is used to take decisions with diagnosis or therapeutic purposes will be classified as class IIa or higher. Many medical apps that provide doctors with a suggestion for a diagnosis are currently classified as class I, but that will change.
Manufacturers of such apps will need to certify their product through a notified body. Since these apps now lack a certificate of a notified body (a declaration of conformity by the manufacturer currently suffices), their conformity has to be assessed in time in order to remain available on the market. Manufacturers will also have to make efforts to gather clinical evidence for the safety and efficacy of their product.
In other categories of medical devices products will be subject to reclassification (typically up), forcing manufacturers to invest time in keeping their products on the market.
Maintenance of medical equipment will be restricted to manufacturer personnel
Fiction
A medical device may only be put into service when duly supplied and properly installed, maintained and used in accordance with its intended purpose (article 5.1). Proper maintenance is a requirement, however, it is not specified who must or may execute these activities.
The manufacturer has the liberty to formulate additional requirements in the manual regarding the required expertise or education of the person who performs the maintenance (annex I.23.4). This provides the manufacturer with the opportunity to set the bar high, either in terms of qualification or costs, up to the point that a hospital is not able to comply. At the same time, a manufacturer risks overpricing his product by doing so. Also, it is to the manufacturer’s advantage that small malfunctions can be dealt with quickly; a service that only trained hospital technicians can provide within a short time frame (and at a reasonable cost).
The manufacturer can also provide instructions on the nature and frequency of the preventive maintenance. The performance and safety of a device during its expected lifetime are the manufacturer’s responsibility to guarantee , provided that the device is maintained according to the instructions (annex 1.6). Deviations from protocol will affect the liability of the manufacturer regarding its device, but the law does not say that it is prohibited. It is the hospital’s responsibility to provide good and safe care to its patients. Modifying the maintenance protocol at least needs justification and a risk assessment.
When a hospital donates medical devices after they have been used or makes them available on the second-hand market, it must comply with the rules set out in the MDR.
Fiction
The MDR is aimed at the protection of patients and consumers, mainly by regulating market access. When devices that already have been put into service are further made available on the market, this does not fall under the rules of the MDR (“Whereas” section, point 3). This does not imply that a hospital in this case does not carry any responsibility for the devices to be sold or donated.
Market access for manufacturers
A manufacturer is obliged to consider alternative treatment options while evaluating its own device.
Fact
Looking at alternative treatment options is a compulsory part of a clinical evaluation (article 61.3). This stimulates a critical evaluation of the new device with for instance current practice, thereby ensuring that new devices will have a higher benefit-risk ratio than devices that are already on the market.
Every new medical device will require a clinical investigation
Fiction
In order to bring a device to the market, a manufacturer has to provide sufficient clinical evidence to prove that its device complies with the general safety and performance requirements. The amount of evidence has to be appropriate for the device and its intended purpose (article 61.1). A clinical evaluation is to be carried out to collect the clinical evidence, comprising of three parts: 1) a critical evaluation of the relevant scientific literature currently available on existing, equivalent devices, 2) a critical evaluation of all the clinical investigations of the device itself and 3) a consideration of currently available alternative treatment options (article 61.3). If part 2 does not yield any results and part 1 and 3 provide sufficient clinical evidence, a clinical investigation is not mandatory. This principle also applies to class III devices and implantable devices. However, demonstrating equivalence for such devices is more difficult. The notified body must confirm the equivalence of the new and current device and will check whether the post-market clinical follow-up studies are appropriate to demonstrate the safety and performance of the new device (article 61.4).
Furthermore, carrying out a clinical investigation may not be appropriate for certain devices (article 61.10). In those cases, conformity can also be demonstrated with non-clinical testing methods, substantiated with arguments by the manufacturer. Validation of diagnostic software can just as well be performed with offline patient data, raising the question whether a clinical investigation is even ethical in such an instance. The same holds for investigating proven technologies such as band aids.
Nevertheless, the MDR does not allow for ‘grandfathering’. Devices placed on the market after May 2020 will not simply be permitted based on equivalence with a device carrying CE-marking under the MDD.
The manufacturer of a high-risk medical device can consult an expert panel before the clinical investigation.
Fact
The manufacturer of a class III medical device or a class IIb product with an integrated drug can consult an expert panel to have the intended strategy for the clinical investigation assessed (article 61.2). The manufacturer must take the panel's opinion into account. Currently, the European Commission and the Medical Devices Coordination Group are preparing the installment of the panels and recently announced that the call for experts will be published later on in 2019. The panels are also designed to contribute to the development of guidance documents, such as common specifications.
A manufacturer can still apply CE-marking for a class I medical device
Fact
When the manufacturer of a class I medical device has prepared the corresponding technical documentation (annexes II and III), he can declare that his product complies with the MDR (article 52.7). However, if the class I device has a measuring function, is delivered sterile or is a reusable surgical instrument, then a conformity assessment by a notified body is required. This assessment is then limited to one of the aforementioned aspects.
A manufacturer who has placed a medical device on the market under the MDD does not have to comply with the MDR during the period in which the corresponding CE certificate is valid
Fiction
A device with a valid CE marking according to the MDD (93/42/EEC) or AIMDD (90/385/EEC) may continue to be sold after May 2020. A number of MDR rules must already be applied by the manufacturer, such as post-market surveillance and registration of the device in Eudamed (article 120.3).
A notified body can force a manufacturer to perform additional clinical investigations after a device has been placed on the market
Fact
When assessing the manufacturer's file, the notified body may conclude that the clinical evidence is insufficient to allow the device to be used for its intended purpose. It can then decide to limit the intended purpose to a specific patient group or prescribe specific post-market studies (article 56.3).
The effectiveness of a medical device must be demonstrated every 5 years through a randomized controlled trial
Fiction
The MDR requires manufacturers to take into account the current state-of-the-art applicable to their device in their clinical evaluation plan. In addition, the post-market surveillance plan must be suitable for keeping the device up-to-date, partly by carrying out post-market studies. As long as results from existing research are applicable, there is no obligation to conduct a new clinical study.
Medical equipment may only be sold to a trained user
Fiction
The MDR spends only a few words on user training. It is certainly not a condition for sale. The competence of the users is not addressed in the MDR either. At the design stage, the manufacturer must take into account the education and training of the intended user of his medical device (annex I.5) and may specify in the instructions for use what specific training or expertise is required (annex I.23.4). As many medical devices are used by patients themselves, it would be a considerable task for a manufacturer or supplier to verify that the user is trained for every device sold. Obviously, a user must be competent when using a device in order to provide good and safe care.
Use and development in the hospital
The clinical evaluation of a medical device intended for home use can be used for the conformity assessment procedure of a new version intended for use in the hospital
Fiction
A device is equivalent if the technical, biological and clinical characteristics are similar to such an extent that there is no clinically significant difference in safety and clinical performance (annex XIV.A.3). The user of the device is a characteristic that must be taken into account when claiming equivalence. When equivalence is not demonstrated, the existing clinical evaluation cannot be used for the new device.
From 2020, hospitals must register all UDI’s of the devices supplied to them
Fiction
The obligation to register and store the UDI’s of the devices supplied to them is limited to class III implantable devices (article 27.9). Member States may extend this obligation to other groups of medical devices in the future.
Every medical device that is used in the treatment of the patient must be registered in the Electronic Patient Records
Fiction
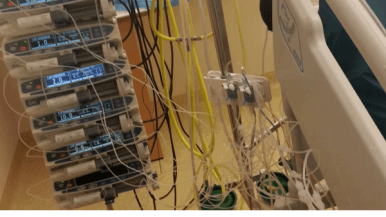
The MDR prescribes healthcare institutions to store the UDI for class III implantable devices (article 27.9) and this obligation can be extended by Member States to other devices. The registration of all medical equipment used in a patient is not mentioned in the MDR. The use of device registers and databanks is encouraged by the European Commission (article 108). A doctor does not, however, have to inform the patient about every patch, infusion pump, monitor, ventilator, operating table, heating mattress, anesthesia device or other material used during an operation.
A device that is tailor-made for an individual patient with a 3D printer is a custom-made medical device
Undecided
So-called computer aided manufacturing techniques, such as 3D printing, laser sintering or stereolithography, are standardized production processes to which quality management is applicable and for which certification is therefore possible. If a medical device can be tailor-made for an individual patient by changing a number of parameters from a standard model, this is not considered to be custom-made (article 2.3). There is still plenty of discussion about this subject within Europe. A special task force is working on this subject and therefore it is still too early to make a conclusive statement about this.
When third-party replacement parts are used, the CE certificate is no longer valid
Fiction
The use of third-party replacement parts is permitted, provided that the manufacturer of these parts ensures that the replacement part does not affect the safety or performance of the device (article 23).
When a medical device is developed in-house by a hospital, the hospital becomes a manufacturer
Fiction
The development of a medical device is not sufficient to qualify as a manufacturer. To become a manufacturer, the device must also be marketed (article 2.30), whether for a fee or free of charge. If the device is not transferred to another legal person, the hospital is not a manufacturer according to the MDR. However, the hospital must then meet the conditions and requirements from article 5.5 and must, among other things, demonstrate that the product meets the general safety and performance requirements.
The instructions for use of an in-house developed medical device must meet the same requirements as the instructions for use of a device available on the market
Fact
The MDR sets rules for healthcare institutions that manufacture a medical device for use within their own institution (article 5.5). One of the requirements is that the device meets the general safety and performance requirements. The instructions for use are part of these requirements and must therefore be drawn up by the healthcare institution according to the same rules set out for manufacturers (annex I.23.4).
Documentation and transparency
In the annual safety report for class IIb and class III medical devices, manufacturers also estimate the extent of the use of the device
Fact
In the context of post-market surveillance, manufacturers must prepare a periodic safety update report (PSUR) for class IIb and III devices annually. Part of this is an indication of the sales volume and an estimate of the size of the population that uses the device (article 86.1 and articles 87, 88 and 89).
A manufacturer does not have to report on non-serious incidents in Eudamed
Fiction
A manufacturer does not have to report a non-serious incident directly to the competent authority or his notified body, but for class II and III devices, the manufacturer must report trends in the periodic safety update report (PSUR) as part of their plan for post-market surveillance (article 88.1). This involves any statistically significant increase in frequency or severity of incidents. The reports on trends and PSUR are processed in Eudamed (article 92.1), so information on non-serious incidents is also reported by manufacturers in Eudamed. It is not yet clear which (part of that) information will be made available to the public (article 92.3).
Post market surveillance will cost hospitals a lot of time
Fiction
The MDR sets stricter requirements for manufacturers to monitor their product after it has been placed on the market. To this end, manufacturers will want to gather more information about the experiences with their products. A manufacturer must prepare a post-market surveillance plan, which specifies which resources are used and how the data is collected (annex III). This includes a continuous review of the benefit-risk ratio and the risk management of the device. In this plan, the manufacturer also determines whether post market clinical follow-up is required.
Professional users and hospitals have a lot of information that could be relevant to PMS, but they have no obligation to provide data to the manufacturer in the context of PMS. Of course, hospitals and professional users have an interest in ensuring that the effectiveness and safety of medical devices is guaranteed. Therefore, they could make agreements with certain manufacturers about the information to be exchanged.
If the UDI-DI of a device is included in the UDI database of Eudamed, this means that the product carries a CE marking
Fiction
The UDI-DI, the unique code to identify a type of medical device, must be registered by the manufacturer in the UDI database of Eudamed. The allocation of the UDI-DI takes place before the device is placed on the market (article 29.1), and therefore the availability of the UDI-DI in the database does not mean that the CE certificate has been issued by the notified body (annex VI.C.5). The FDA uses the same identification system, so a device available in the United States may already have a UDI-DI.
All EU citizens will be able to consult a summary of the safety and performance of each medical device online
Fiction
Eudamed is the European database where all relevant information about medical devices will be stored. Part of that information will also be made available to the public, such as a summary of safety and clinical performance (article 32). However, only implantable devices and class III devices must be provided with such a summary. For other resources, the basic data elements from annex VI, Part B, will be publicly available through Eudamed. This includes, for example, the risk class, contraindications, sterility, basic UDI-DI and the manufacturer's name and address.
A patient information leaflet is mandatory for every medical device
Fiction
Patients with an implanted device receive information from the healthcare institution about the device, including the implant card, prepared by the manufacturer (article 18). This implant card is not applicable for devices such as plates, screws, fillings, stitches, etc.
In the instructions for use, the manufacturer can state information such as residual risks or contraindications that must be communicated to the patient (annex I.23.4.g) and alert the user and / or patient that all serious events with the device must be reported to the manufacturer and the competent authority (annex I.23.4.z).